

Modern Provider Network Management
Effective Provider Network Management is essential to delivering value and ensuring crucial services are seamless and uninterrupted.
Watch the On-Demand WebinarAs the healthcare industry continues to see a rise in healthcare consumerism, patient loyalty is increasingly important to health plans — otherwise, members are likely to search for a new provider or change networks. To build patient loyalty, payors, and providers are looking to adopt the value-based healthcare model. This model seeks to improve individual patient care and population health management as well as to increase efficiencies and reduce costs.
One of the essential steps for a payor to enable value-based patient care is effective provider management. Attracting and retaining the best providers to your network, and supporting them however possible, helps promote patient-provider communication and ensure improved clinical outcomes leading to quality ratings, better member retention, and greater overall efficiency.
However, outdated business systems and homegrown solutions can complicate provider data management and hinder how effective payors can be with their provider network management (PNM). Payors today need modern PNM systems in place that allow them to not only better manage their provider networks but also to serve their members better.
What Is Provider Management?
Provider management or provider network management (PNM) is how health plans (payors) can support the relationship with providers/physicians. Good PNM is achieved by leveraging fully integrated, technology-enabled services, coupled with modernized processes and effective data management to excel in providing support for the following areas:
- On-boarding
- Credentialing
- Enrollments
- Privileging
- Appointments
- FPPE/OPPE
- Quality Improvement
- Risk Management
PNM is built on the goals of streamlining communication, building strong relationships, and aligning providers with their organization’s values, vision, and mission. The ultimate goal is to continuously improve the quality of care and the overall member experience.
Why Is Provider Management Important?
Provider management in healthcare directly affects patient satisfaction, which has been defined as how the healthcare service or product is regarded as “useful, effective, or beneficial” by a patient. Simply put, if patients aren’t satisfied with the quality of care, they’re likely to seek out new providers or new health plans.
A study by Milliman found health plans with the highest star ratings from the Centers for Medicare and Medicaid Services made effective provider management part of their best practices. Those higher-rated plans employed “oversight, collaboration, contractual performance measures, and incentives” for their healthcare provider management. Concurrently, plans with higher star ratings attract and retain more members than lower-rated plans.
Other impacts of PNM include:
- Ensuring alignment to appropriate regulations, bylaws, and desired organizational outcomes
- Avoiding fines and penalties for failing to correct erroneous or out-of-date provider information
- Reducing the risk of liability if a member claims that poor management, lack of communication, or incorrect data contributed to poor service or care
Good provider management is essential not just for improving the patient experience. It also plays a critical role in the total experience — a consideration of the combined patient/customer, provider, user, and employee experience across multiple platforms — which Gartner spotlighted as a top trend for U.S. healthcare payors in 2022.
Benefits of Provider Management
The availability of high-quality, patient-centered, value-based healthcare is at the top of mind for today’s health plan members. As a payor, a well-cultivated and supported network of providers is a competitive advantage — the better you can manage your network, the better they can provide care for your members.
Effective PNM makes it easier for your providers and keeps them happy, resulting in a greater chance of retention for skilled providers. High levels of effective provider management have been correlated to:
- A more streamlined onboarding process
- Optimized revenue management
- Reduced administrative redundancy
- Improved provider engagement and retention
- Simplified compliance reporting
- Proactive risk management
- Standardized performance evaluations and peer review processes
Provider Management Best Practices
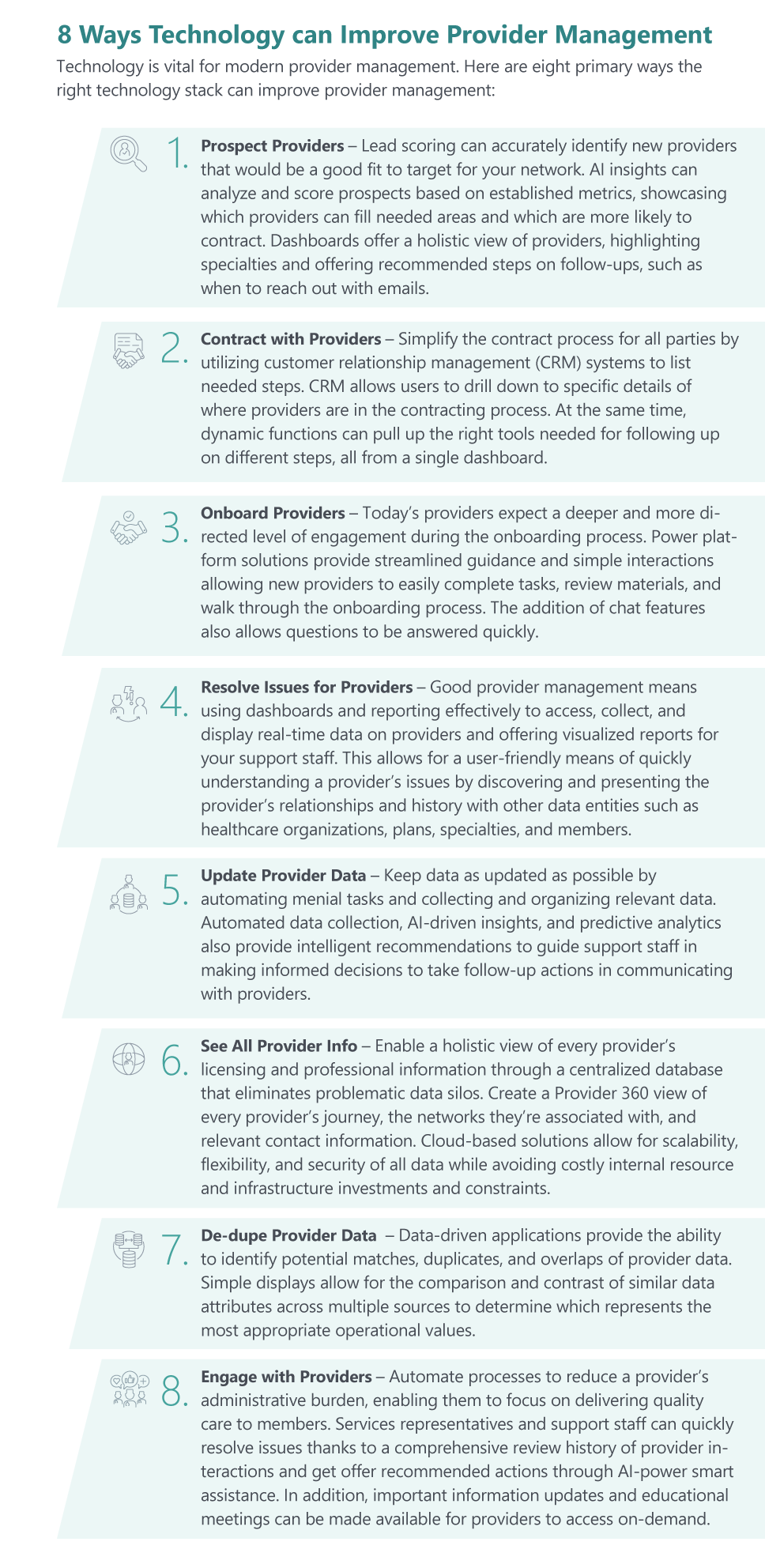
Effective provider management requires consistent communication. Payors must share a clear vision with specific goals while gathering the latest data to inform their insights and proactively address issues. PNM starts by leveraging intuitive technology with data-driven insights to enable the following best practices:
- Unify and enrich data — It is important to match, reconcile, and merge similar data from across multiple third-party sources to create a single, reliable source of truth of provider profiles. This is the most effective way to reduce errors and oversights.
- Provide a consistent experience across all channels — Not only should the primary management system receive reliable and relevant data, but that same accuracy should also apply to every downstream system and application. No matter how or where your employees and providers access the data, everyone should have the same experience.
- Predict provider intent — Be better prepared to effectively support providers by analyzing data for insights. For example, a better understanding of practice patterns, costs, outcomes, network capacity, and fitness to the membership base can provide support where it’s most needed.
- Proactively target and engage providers — Support providers through regular, targeted outreach to remind them of important milestones and encourage participation in relevant programs. Encourage their development — and forge stronger relationships — by offering training and assistance informed by decision support and data-driven insights.
- Intuitive self-service — Give providers the freedom to access information when and where they need it. Utilize web portals and mobile apps to allow them to connect from anywhere. Even allowing them to converse with chatbots can help reduce wait times and increase efficiencies.
Challenges in Managing Providers
Following best practices may be the goal, but the reality is getting to that point requires the right processes, supported by the right tools, to meet and overcome challenges. While every industry faces challenges in managing employees and contractors, the healthcare industry has challenges unique to payors and provider data management:
- Patients may see multiple healthcare providers throughout their treatment. Each provider could be utilizing different systems for storing and processing clinical data, health records, and other relevant provider network data. Health plans need to have ways of integrating and organizing these siloes of disparate data. Otherwise, they risk negatively impacting their analytics and reporting, which reduces the efficacy of providers’ efforts to improve overall performance, reduce errors, or improve finances.
- There can be uncertainty in determining what data can be collected and how to collect and organize it. In addition, certain unique situations, such as where providers are seeing patients from different states, can lead to complications or oversights in collecting data. For example, inefficient manual workarounds can result in data loss, inconsistent formatting, and the replicating or “duping” of data.
- Overall, a lack of data integration and management can frustrate providers, damaging the payor-provider relationships. This often happens following mergers and acquisitions, where payors must integrate data from multiple disparate systems and need to find ways to consolidate information quickly and efficiently. Excessive delays may hinder a payor’s ability to differentiate itself in the marketplace and decrease member satisfaction.
- Outdated technology or the inability to quickly update data will lead to inaccuracies in all areas — from member information to practitioner credentials and contact information to changes to health plans or affiliations. Transitioning from paper-based workflows to more modern digital systems is essential for real-time communication, information sharing, and allowing for a more streamlined patient experience. Perhaps the most significant challenge payors have is determining how to make that digital transformation.
A modern PNM process allows for more accessible interactions, faster actions, and more comprehensive views of everything relevant to your providers. Effective provider management can lead to more accurate provider directories, support more accurate claim payments, decrease compliance transgressions, and improve member and provider satisfaction. Most importantly, when you can provide them with more effective support, you’re better able to close any gaps in care for your members.
Improve Provider Management with Hitachi Solutions
Data must support any modern provider management solution if it’s to be accurate and up-to-date and easily accessed if it’s to be useful.
Hitachi Solutions enables health plans to confidently achieve their provider management goals with the support of Microsoft-powered solutions. Dynamics 365, Microsoft Cloud for Healthcare, and Hitachi Solutions’ healthcare provider management solutions make it possible to develop automated care coordination workflows based on custom triggers and requirements.
If you are ready to modernize your provider management capabilities, check out our on-demand webinar or contact us today.


