Enhance member experiences with personalized service
Download the free DatasheetHitachi Solutions Engage for Health Plans
Enhance Member Experiences with Personalized Service


Improve member engagement
Choosing a health plan is a big life decision — one that involves handing over sensitive medical information and putting full faith in the insurer of choice. As a result, health plan members are demanding a higher level of service and a more engaging member experience, leaving insurers and health plans to look for ways to improve member engagement and long-term member loyalty.
With Dynamics 365, we can build a single view into the heartbeat of every member, while we deliver more interoperability to providers, partners, members, and employees.
Michael Della Villa, Chief Information Officer, MVP Health Care

Purpose-Built Relationship Management for Health Plans
Hitachi Solutions Engage for Health Plans offers payors a practical solution to effectively manage and foster profitable relationships across agencies, members, brokers, and other partners. Our solution enables you to focus on all aspects of your business and the member lifecycle, from relationship and engagement management to business development.
Engage for Health Plans enables organizations to:
- Streamline the onboarding process from start to finish
- View current and historical plan information, agency performance metrics, and upcoming activities
- Identify those with unmet insurance needs using rich analysis and segmentation tools
- Foster stronger relationships across members, agencies, brokers, and third-party partners
Engage Everyone in the Process
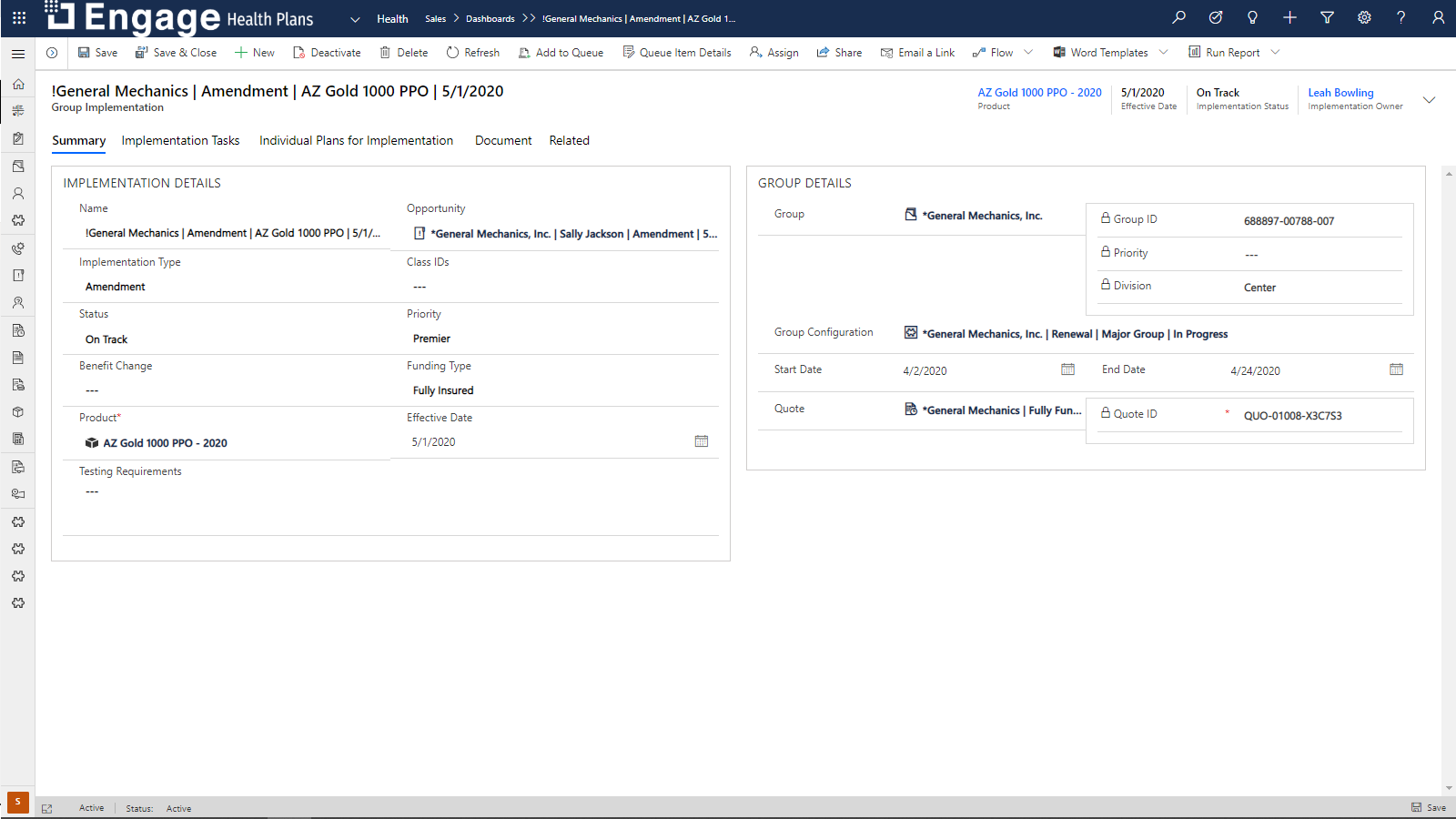
Process plan onboarding and renewals quickly and efficiently, giving full visibility into the process and clear next actions to drive completion. Give health plan administrators a comprehensive end to-end platform for managing onboarding and renewals that engages everyone.
- Group Segmentation: Better understand your customers and use data points such as company, organization, division, and plan details.
- Onboarding and Renewal Management: Automatically create, assign, and track all tasks and information associated with plan onboarding.
- Implementation Management: Automate implementation to increase efficiency and capture changes with ease.
- Report Automation, Summary of Benefits: Automatically create documentation to save time and ensure accuracy.
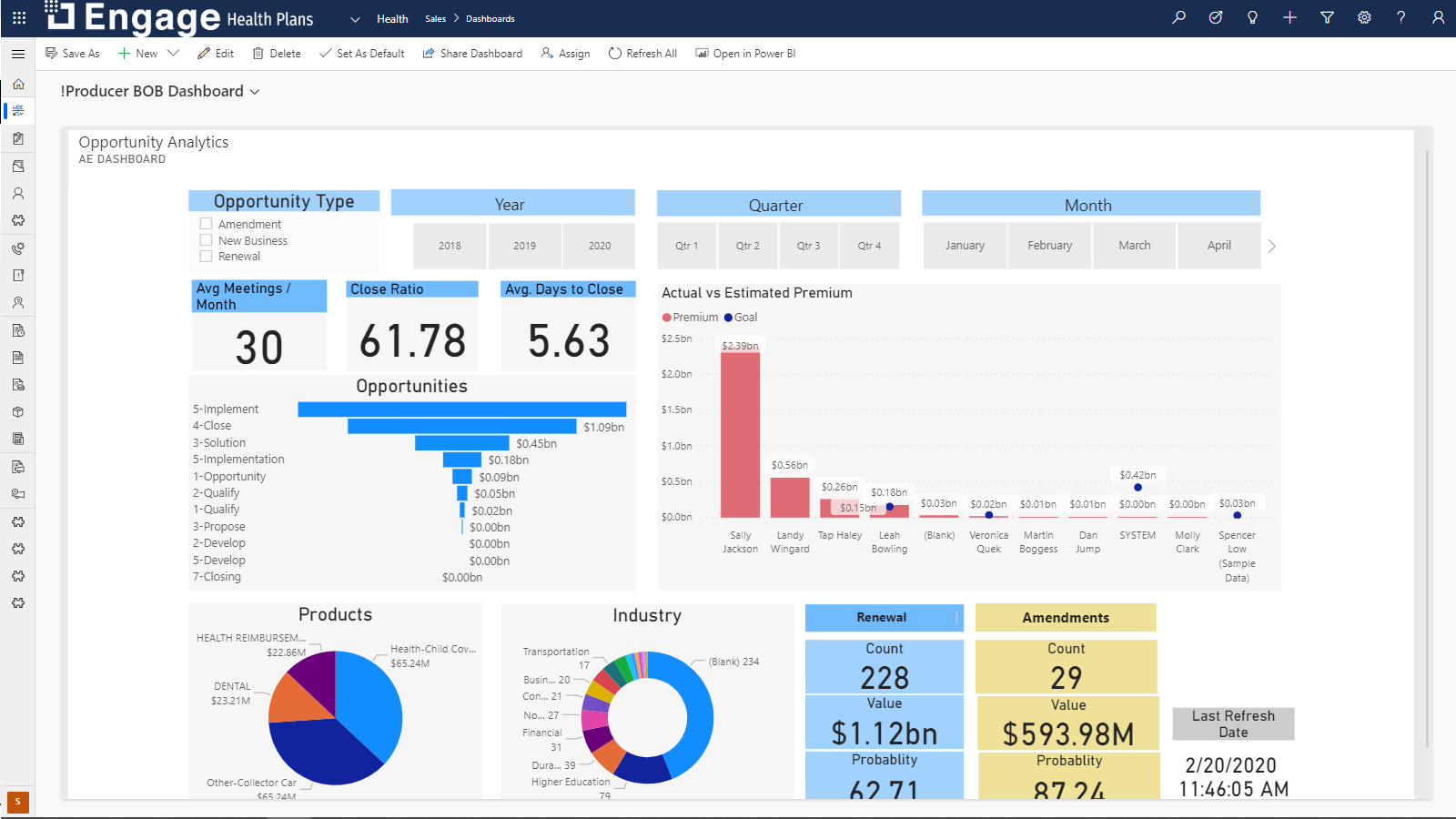
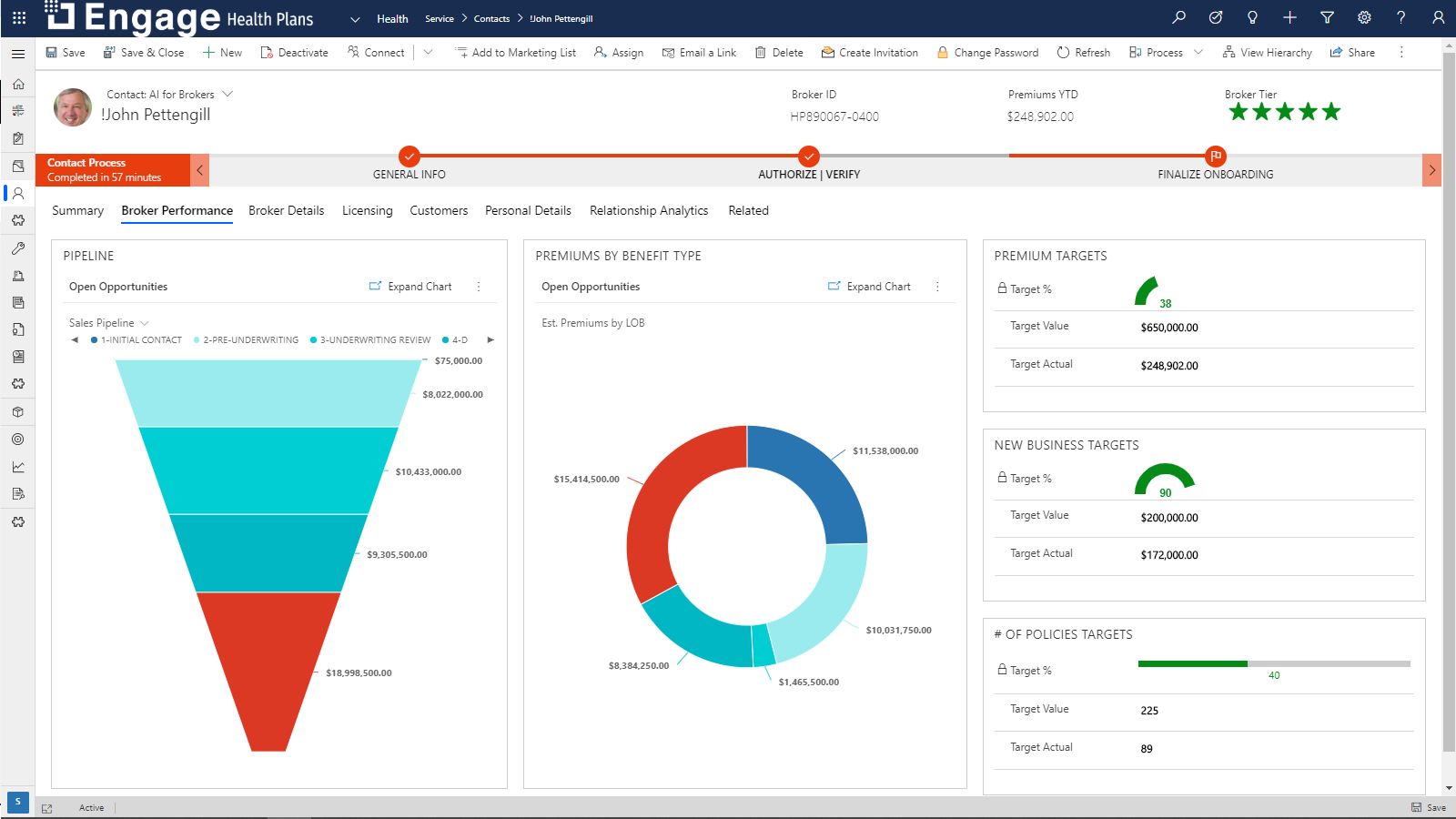
Execute Better Across the Entire Quote-To-Card Lifecycle
Allows you to provide superior transactions and engagements, every time. The solution gives you a holistic view of all data from one system, consolidates the entire process into a single automated workflow, personalizes and speeds interactions, and integrates across all channels. It also provides dashboards, performance management, and automated tasks to help you execute better across the entire quote to card lifecycle.
- Opportunity Management: Identify and execute on sales opportunities with better collaboration, tracking, and process management.
- Group and Individual Segmentation: Grow premium by zeroing in on good leads.
- Lead Management: Ensure consistent lead follow-up with automated interactions.
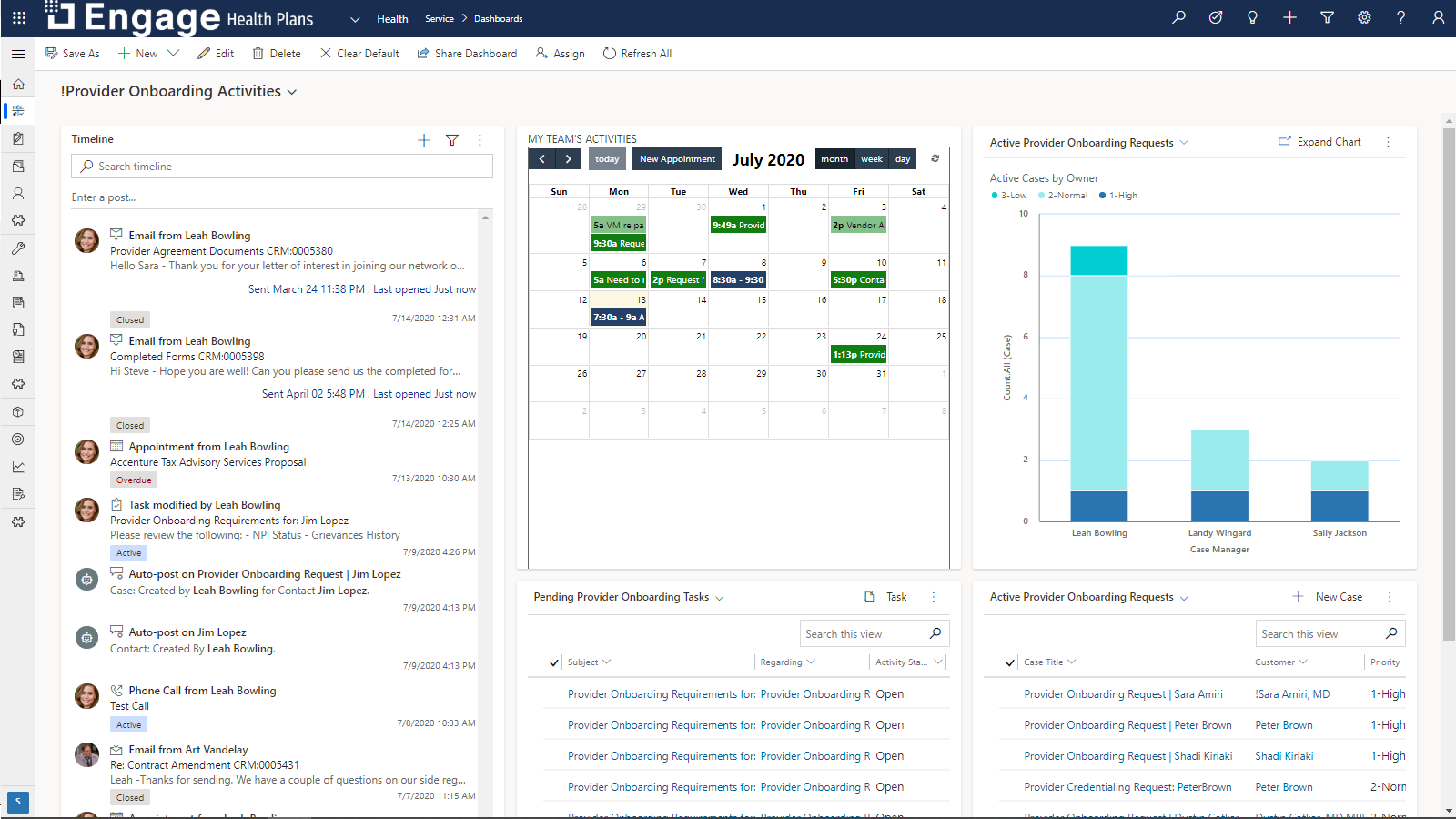
Get Visibility into Provider Organizations
Store, represent, and manage all the complexities in provider information and relationships. Gain visibility into provider organizations, including basic organization details, activities, and grievance management.
- Provider 360: Improve member and provider satisfaction with access to better information to support alignment between members and providers.
- Provider Calls and Visits: Foster consistent and productive provider engagement with intuitive planning, best practices, and reporting tools.
- Grievance Management: Give providers reliable information about member grievances and improve response time for providers and members.
Put data to work
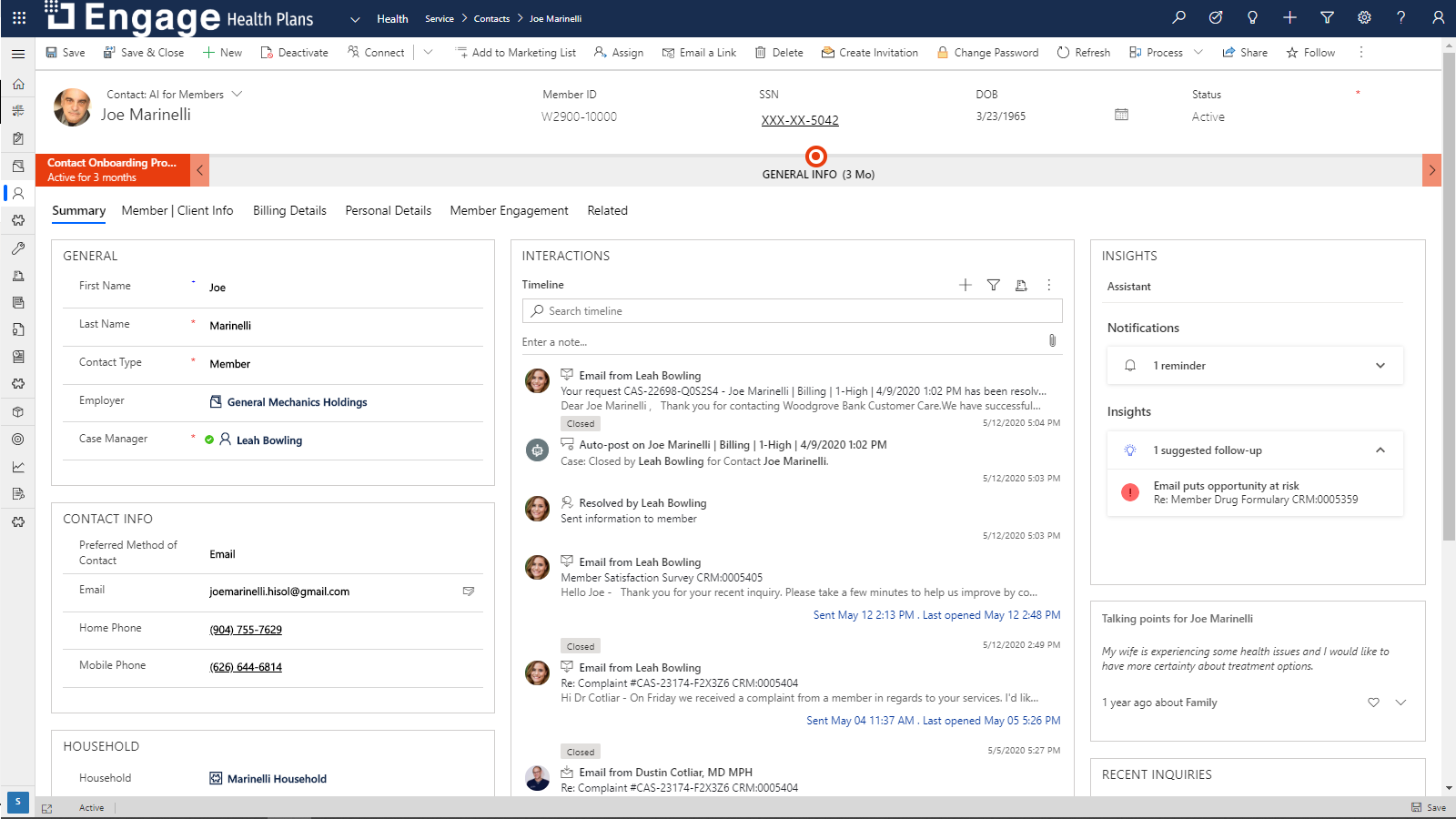
Establish a true 360-degree view of each member by rapidly integrating disparate systems in accordance with industry best practices. Aggregate member and plan data from policy administration, claims, billing, imaging, document management, and other systems.
- Patient/Member Experience: enable customers to access their medical information and health plan benefits.
- Search and Automation: smart search capabilities help patients/ members locate the information they need instantly.
- Integration with Health and Payor Systems: patients/members can submit issues and get answers to their questions.
Promote Greater Ease of Doing Business
Make it easier for your distributors to work with you and turn the strength of your distributor relationships into a powerful competitive differentiator. Provide performance management and superior visibility into your distributor network, along with tools that promote collaboration.
- Agent, Broker Performance Management: Improve visibility into distributor performance, such as goals and submissions, to unlock new opportunities
- Agent, Broker Sales Plans and Call Reports: Gain a complete understanding of performance metrics, interaction history, and recommended actions
- Agent/Broker Portal: Find and share information, stay connected, and work to achieve desired outcomes
- Interaction Journal: Track interactions with distributors to monitor and gain insight into relationship history
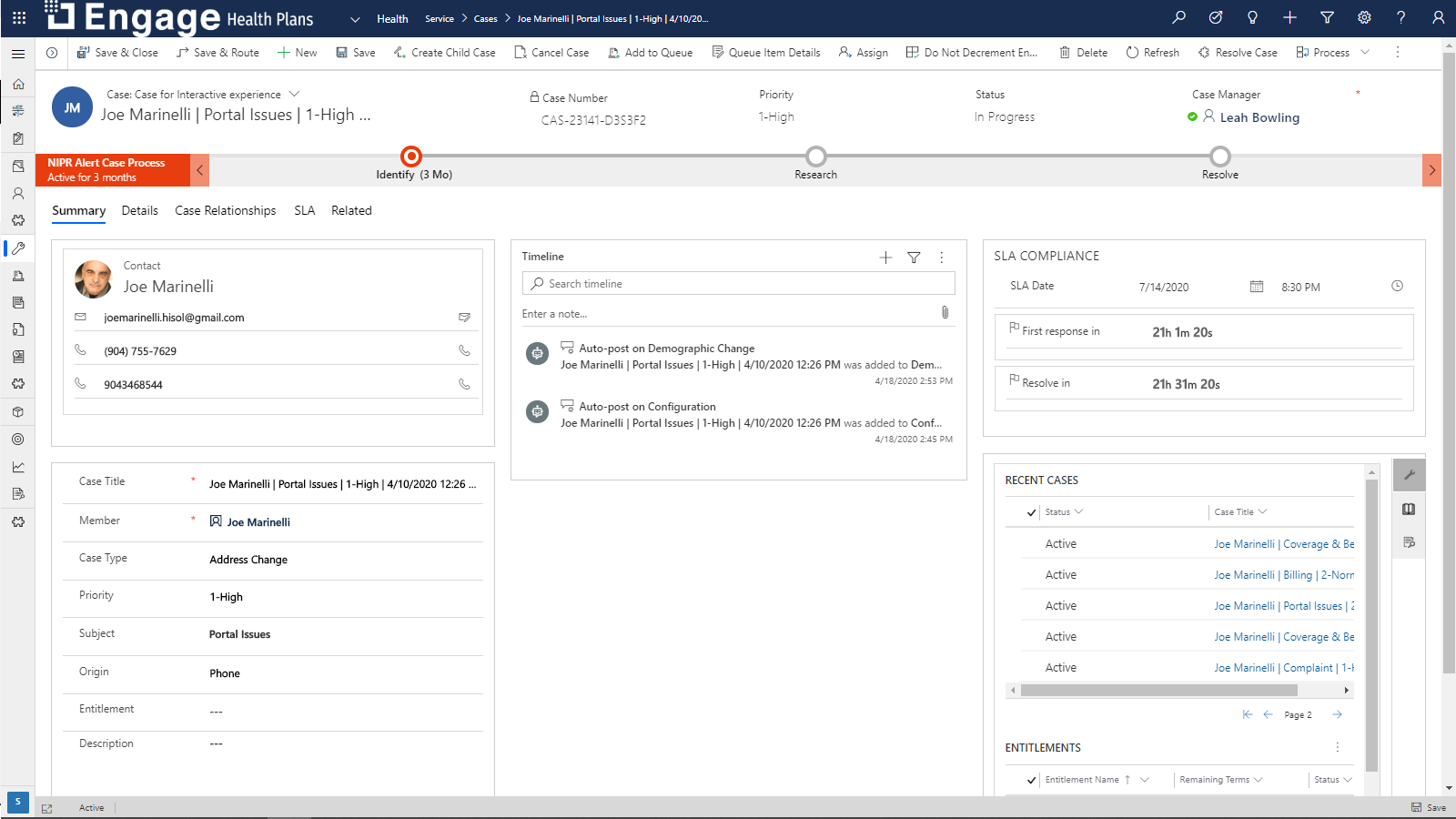
Provide Better Service
Deliver superior member services by giving everyone a complete view of member information along with intuitive service tools. Provide better service in the call center and manage interactions across service, marketing, billing and all other touchpoints.
- Member 360: Get a complete view of member data so you can communicate the right message at the right time and quickly resolve service requests
- Telephony Integration and Call Center Console: Give call center agents a consolidated desktop that displays health insurance payer information, service apps, and guidance for every service call
- Case Management: Improve resolution by capturing customer information and efficiently managing cases from end to end

We’re Here to Help
Enhance your health plan services with our Dynamics 365 add-ons, built on decades of industry and technology expertise. Talk to an expert today.
Contact Us