

Health Plans Scenario Guidebook
Know your industry and unlock opportunities to transform member/patient/provider/broker experiences.
Download the EbookTop Provider 360 Benefits & 6 Must-Have Features
In a market as commodified as health care, competition between health plans is fierce and individual members are often left anxious and confused about their options. As the New York Times noted, even renowned economists are often lost in choosing their health plans.
Members want and need more information, but according to a 2021 J.D. Power study, member satisfaction with provided information and communication was the lowest-performing metric with Medicare Advantage plans. A second study on commercial health plans found that, while health plans had an increasing level of contact with Gen Y and Gen Z members, more than one-third (37%) of all health plan members felt they had no engagement with their health plan, including nearly half (44%) of the Baby Boomer generation.
How can health plans do better for their members? While there are general recommendations on how to increase member engagement, one of the best ways for a health plan to support and attract members is by enhancing its relationship with its healthcare providers.
The strength of the network of providers that a health plan offers is paramount to the retention of existing members and attracting new ones. At the same time, there’s a sentiment in the industry that members will tend to be more loyal to their provider (doctor) than their health plan. Health plans that want to be marketable to new and returning members need to have a comprehensive view of the background, activities, and issues related to their associated health care providers — a provider 360 view.
What Is a Provider 360-Degree View?
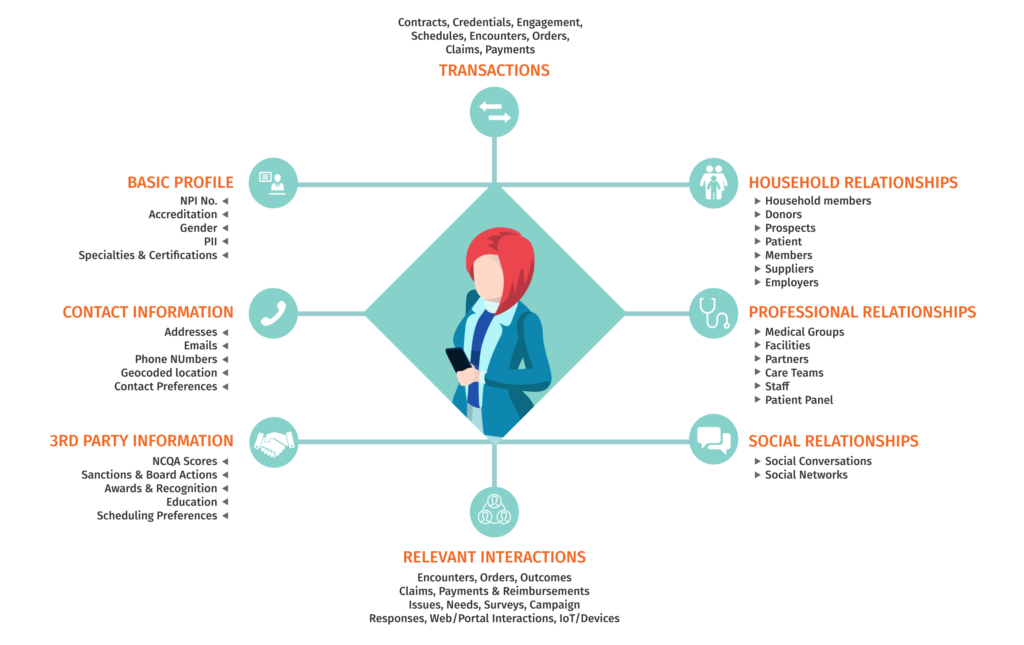
A provider 360-degree view refers to a comprehensive collection of all provider data that is generated throughout the provider management lifecycle, ranging from federal and state medical licensing to enumeration agencies and covering credentialing, history, complaints, billing, and more.
However, just having access to this data isn’t enough — to gain a truly 360-degree view, health plans/payors need to ensure that all provider data they have on hand is accurate and up to date. Navigating the vast array of obsolete data, incomplete records, duplicate entries, and fraudulent information can be extremely challenging considering the large number of databases operated by third-party sources.
Having the capability of accessing all of these different data points throughout the provider–health plan lifecycle is essential for developing and maintaining a true provider 360 view.
Why Health Plans Need a Comprehensive View of Providers: The Provider Lifecycle
First and foremost, having the most up-to-date and relevant information about providers is essential in gaining a competitive edge over other health plans and providing the best possible level of service to members. It has been shown that providers who are supported and more engaged result in improved efficiency, job satisfaction, patient satisfaction, and overall performance.
This level of support is important for the entire lifecycle of the provider–health plan relationship:
Outreach
The first step in the provider lifecycle involves adding new practitioners to the provider network. To inform its outreach, the health plan requires accurate data to know which providers to contact and how best to market to them. In this process, a health plan will run a network adequacy report based on a specific metric, such as geographic area, to determine which services are being requested by members and which specialties are missing. Having a provider 360 view will determine which available providers can best fill in those gaps in care, directing the outreach.
Onboarding
The second step means ensuring that the onboarding process is seamless. This required collecting elements such as the National Provider Identification (NPI) provided by the National Plan & Provider Enumeration System (NPPES) for individual practitioners as well as their associated organizations. Health plans will also need to gather information to perform a thorough background check, which can include details such as a provider’s social security number, required liability insurance, tax identification number, pending lawsuits, and any filed complaints or grievances.
Servicing
Informed servicing is essential to the retention of valued providers within the network. Once the provider is part of the network, a provider 360 view will ensure that the health plan has a full view of their activity and their relationship to plan members. This is especially important in resolving matters of billing or claims. As a provider sends in a list of billing codes to the insurance plan, the health plan needs regular updates on the back-and-forth over the necessity or validity of different prescriptions and procedures. Having one, single point of access to this information enables the health plan to stay on top of other service issues such as required training, updated certification, or problems that need to be resolved.
Termination
Finally, the information from a provider 360 view will aid the health plan in determining whether to retain the services of a provider or end the relationship. Should there be repeated complaints from members or other issues and problems that continually arise, the health plan has the documentation it needs to act. In the case where it is the provider who decides to leave the network, it’s important to have all relevant data available in the case of future inquiries about the time the provider was part of the network.
Why Health Plans Need a Comprehensive View of Providers: Major Benefits
Beyond being able to better manage the provider–health plan lifecycle, there are several general benefits, all of which underscore the importance of developing a 360-degree view of providers:
- As a single point of access for a provider’s services team, a provider 360 view helps to prevent service interruptions. There’s no need to chase down outside information or to do research to answer questions or resolve issues. Instead, the relevant information is available right at the fingertips of any health plan employee.
- Health plans can develop a greater understanding of potential providers, as they may have affiliations and admitting rights with multiple hospital systems. A provider 360 view enables health plans to better track provider relationships with medical groups, health plan products, networks, and members. Maintaining up-to-date and accurate records of providers and services is also easier to better attract and retain members.
- A provider 360 view can enhance plan performance through improvements such as a more efficient and accurate credentialing process, a shorter turnaround time for responding to providers, and the ability to assist in resolving technical issues or claim disputes. Being more responsive can help build a positive payor-provider relationship, resulting in improved provider engagement.
- With a single point of contact, a provider 360 solution enables health plans to streamline various processes, including claims, authorizations, and credentialing. In coordination with the right technology stack, plans can also automate processes for prior authorizations to avoid delays in specialized procedures and referrals.
- Having a more detailed view of the formal and often complicated process of filing complaints or grievances against practitioners, especially with plans like Medicare Advantage, allows for more efficient and accurate communication. This improves the provider network transparency for members while delivering important notifications for providers who may wish to appeal.
- A provider 360 view enables a health plan to see which group is licensing a practitioner and which specific services that practitioner is licensed to provide. Additionally, increased access to more current information enables the plan to accurately model levels of value-based care and improve claim accuracy. Both benefits are greatly helpful in reducing the risk of fraud.
- Having an accurate record of the roster of the current providers makes it easier for members to search for specific care providers. This greater access to information, in addition to increased provider engagement, results in the optimization of members’ health outcomes.
See how digital technology can help health plans create more value for members
Get the Ebook6 Must-Have Features in a Provider 360 Solutions
In order to gain a provider 360 view and its associated benefits, health plans need to look for specific features and functionalities when seeking out a provider management solution. The six most important features to look for include:
- Data consolidation — This is the capability to unify data from disparate systems to provide a comprehensive view of providers and provider relationships, all in one easily accessible, centralized location.
- Automation — Lots of data requires lots of data entry and retrieval. Automated processes streamline many lengthy, complicated processes such as credentialing and prior authorization.
- Reporting tools — One of the keys to achieving a provider 360 view is to generate accurate, up-to-the-minute reports. Being able to rely upon generated data is the basis for improved provider communications and increased engagement.
- Real-time monitoring — Updates happen all the time, so it’s important to be aware when anything critical arises, especially when operating overnight or across different time zones. Real-time monitoring is key for tracking health plan utilization across providers to determine if services are being prescribed appropriately and claims are submitted accurately.
- Advanced analytics —Rather than just learn about what has happened, health plans can utilize data to understand why things happen, and how to plan for future trends. Artificial intelligence can analyze the available data to examine rejections, errors, and other bottlenecks or pain points to pinpoint causes and offer strategies to proactively resolve issues.
- Relationship management — Having a better understanding of providers enables health plans to engage in more targeted marketing. Tools and features that enable communication and outreach will aid in attracting prospective providers and improve outreach to current providers within the network.
Putting together the right combination of features can improve relationships, boost retention, lower costs, and drive efficiencies. However, understanding how to develop a complete digital solution, as well as how to keep it updated, accurate, and complete can be challenging. To establish a true 360-degree view for providers and members, look for a partner like Hitachi Solutions.
Gain Greater Visibility with Hitachi Solutions
A provider 360 view is just one element of Hitachi Solutions’ Engage for Health Plans Provider Services, a powerful complement to Microsoft Dynamics 365 and the Microsoft Cloud for Healthcare.
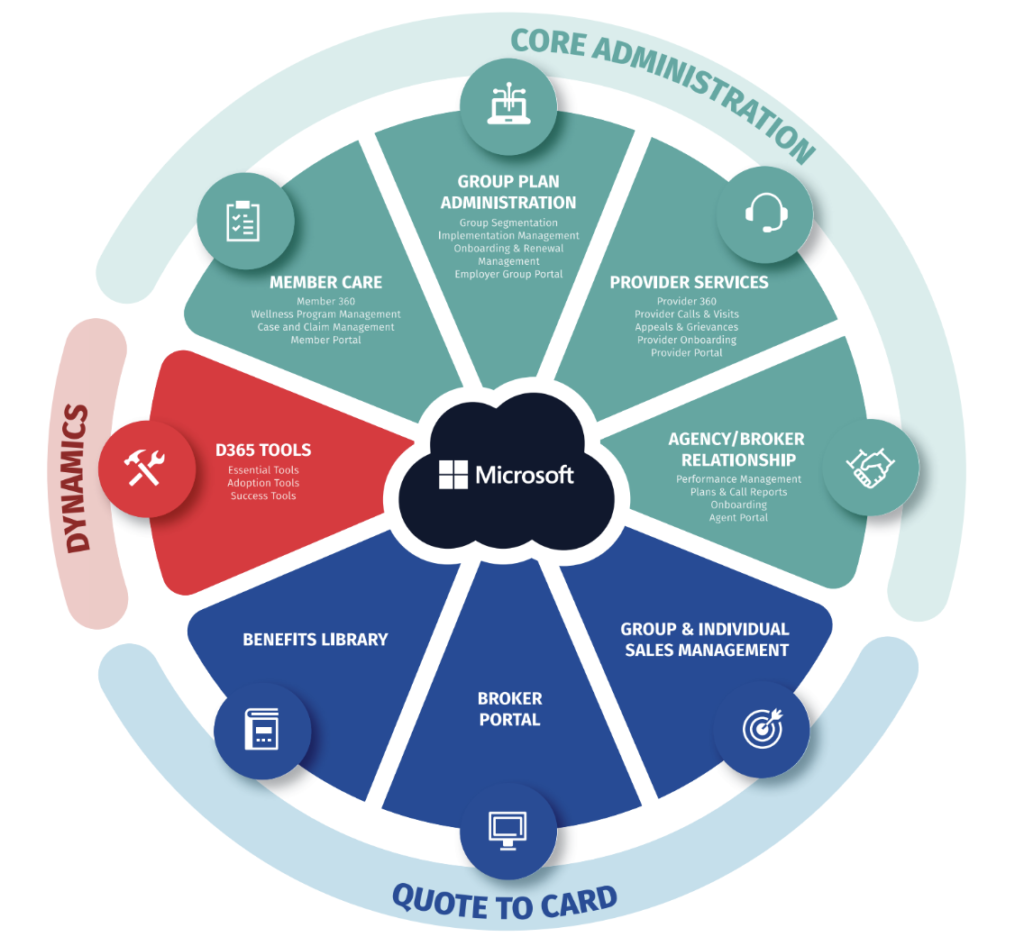
To learn more, download our Engage for Health Plans data sheet to see how you can store, manage, share, and communicate your data in order to grow your network of providers and provide superior member services.
For more information on how we can help you achieve a digital transformation of your provider data management, contact Hitachi Solutions’ team of experts.


